Large-scale in-person simulation training has many logistical challenges. Time constraints and scheduling conflicts often make sessions few and far between, and do not allow for practice and reinforcement. Administrative hurdles and the resource-intensity of the learning method prevent frequent practice, limiting the impact of simulation on improving performance where the rubber meets the road — quality care.
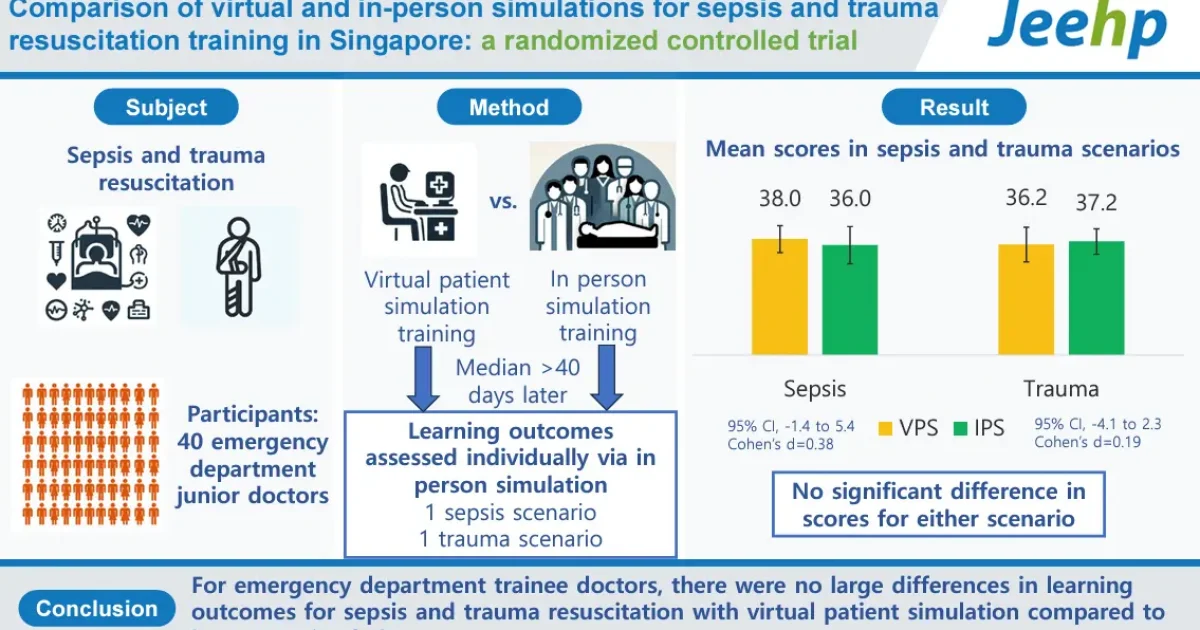
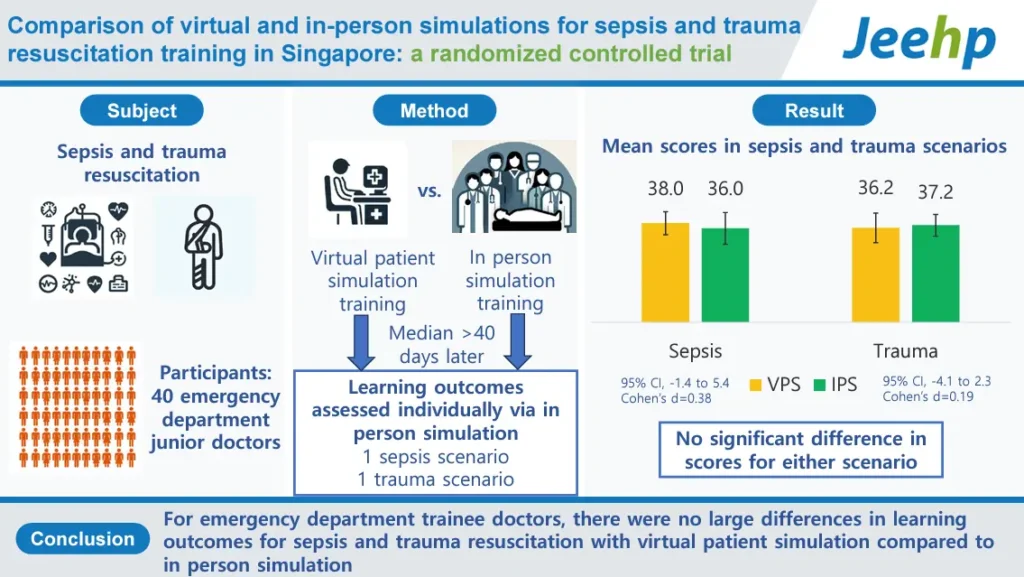
Full Code is an evidence-based educational platform that provides all the cognitive benefits of simulation without the time, space, staffing, and scheduling constraints of in-person simulation. A recent randomized controlled trial compared cognitive, non-cognitive, and overall learning outcomes for resuscitation skills in novices with virtual patient simulation (VPS) versus in-person simulation (IPS).
Low et al demonstrated that the Full Code platform was equivalent to in-person simulation training, firmly establishing the construct validity and educational equivalence of the Full Code platform to mannikin-based simulation.
Learning outcome assessment was conducted using two simulated resuscitation scenarios in a simulation laboratory with a high-fidelity mannequin (Sim-Man 3G, Laerdal Medical). The scenarios covered resuscitation in trauma (hemorrhagic shock from pelvic fracture and splenic rupture) and sepsis (severe bacterial pneumonia with septic shock).
There was no significant difference in overall learning outcomes between virtual patient simulation (VPS) and in-person simulation (IPS) for both sepsis and trauma resuscitation scenarios in both cognitive and non-cognitive skills assessment, underscoring the value of VPS in increasing the scope and depth of simulation training when added to a medical education curriculum.
The outcomes we measure in Full Code are the same ones we assess in the sim lab or clinical learning environment: stabilization, diagnostics, interventions, reassessment, systems-based practice, and others relevant to patient care. The platform tracks every action, so the data we can provide on individual performance is highly granular evidence of one’s current competency level.
Each case only takes a few minutes to play and requires no dedicated staff or equipment. At the heart of deliberate practice is repetition. In the sim lab, you can only cover a fraction of clinical practice, often with learners who diffuse the experience across the group so you cannot really teach to individual deficits. Full Code enables learners to repeat simulations to refine and consolidate concepts, as well as refresh and reinforce concepts with spaced repetition to fight knowledge decay.
With repetition, learners can track their performance improvement independently as they explore the library of cases we have designed. Individuals can “rapid-cycle” learning and identify exactly where they need to focus their study to improve patient care. Based on the best evidence in educational theory and practice — including the Kolb learning cycle, spaced repetition, and deliberate practice — learners can garner granular performance feedback on clinical competencies independently without fear of judgment.
In addition, Full Code is situated learning; students learn as they perform the same cognitive tasks required for patient care in an applied setting. For medical educators, the Full Code dashboard provides granular feedback on each learner with detailed performance assessments. From diagnosis and management to disposition, you can see your learners’ clinical reasoning evolve.
Our mission is to make simulation training available to every clinician regardless of access to an academic medical center or simulation lab. All that’s required is a smartphone. Whether working in an urban, rural, or a remote setting, clinicians and their patients deserve the best evidence-based cognitive training possible. Full Code can deliver that anywhere, anytime. Our goal is to not only improve education for individuals, but to increase the consistency and quality of medical practice globally.
Reference:
Low MJW, Chan GWH, Li Z, Koh Y, Jen CL, Lee ZY, Cheng LTW. Comparison of virtual and in-person simulations for sepsis and trauma resuscitation training in Singapore: a randomized controlled trial. J Educ Eval Health Prof. 2024;21:33. doi:10.3352/jeehp.2024.21.33. Epub 2024 Nov 18. PMID: 39552082